A deadly virus with no cure has spread to Europe for the first time...And virologists everywhere are worried

Oropouche virus has been detected in Spain, Italy and Germany
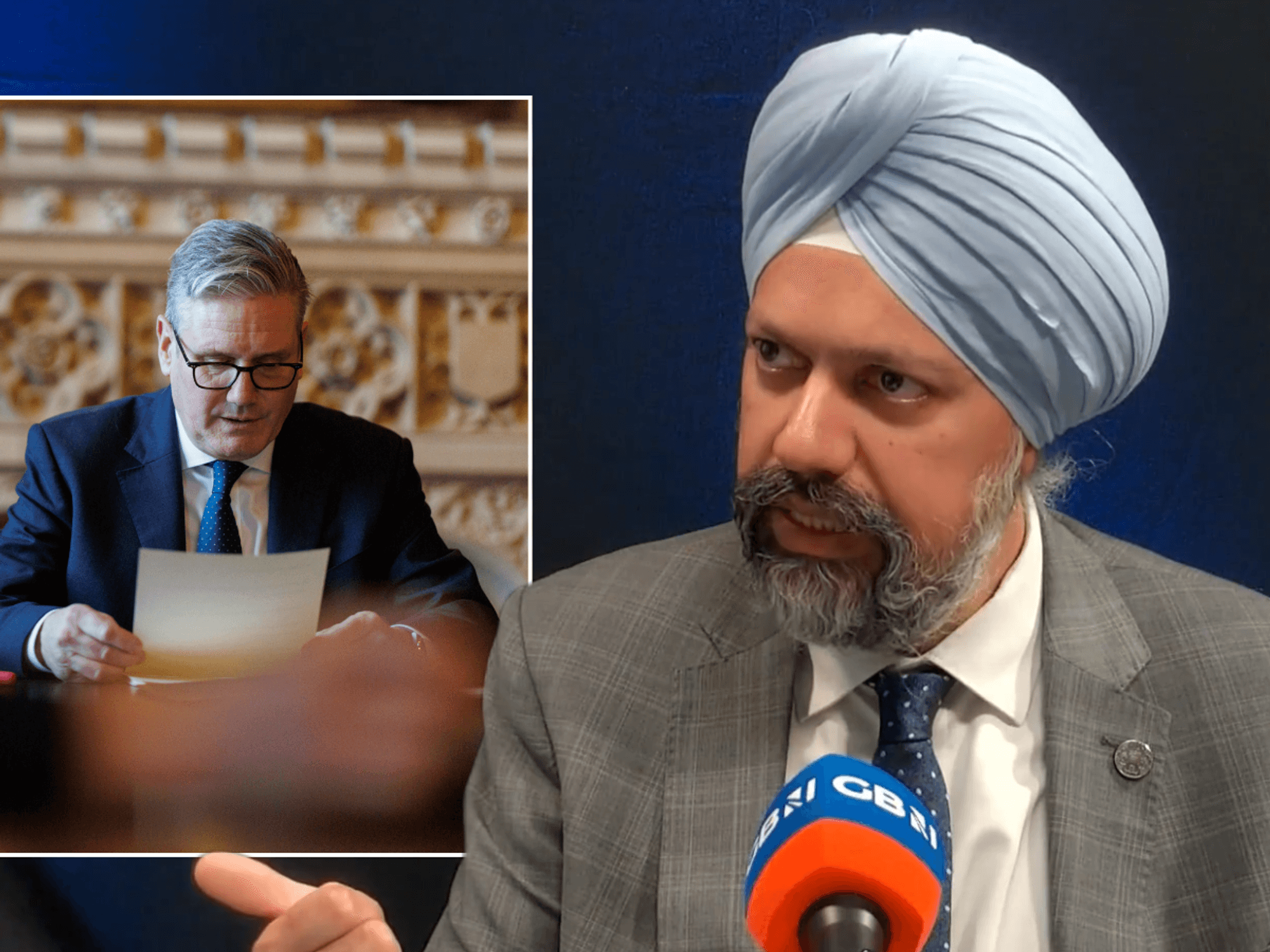
|Getty Images/Grok

It come after health authorities confirmed the first deaths from Oropouche virus in July
Don't Miss
Most Read
Latest
A mysterious virus endemic in parts of South America is spreading outside the region for the first time - and it's concerning virologists.
For decades, Oropouche virus was confined to areas close to the Amazon. The first human case was discovered in the village of Oropouche in Trinidad and Tobago in 1955.
Five years later, the virus was detected in Brazil from a blood sample taken from a sloth. This is why it's sometimes referred to as "sloth fever".
Since then, there have been intermittent outbreaks in humans, but they have all been confined to forested areas, such as the Amazonas.
The vector-borne virus has historically spread to humans via midges and no human-to-human contact has been established.
Cases have tended to be mild, producing symptoms similar to other arboviruses, such as dengue fever.
Patients typically present with fever, headache, and muscle or joint pain, and recover after one to two weeks.

The virus was detected in Brazil from a blood sample taken from a sloth
| Getty ImagesThat bubble has now burst
The virus is changing on all three fronts.
Let's start with transmission.
Oropouche virus is surging in regions where it is endemic. It is also turning up in new environments.
More than 8,000 human infections have been confirmed in the Americas this year alone, mostly in Brazil but also in Peru, Bolivia, Colombia and Cuba.
Imported cases have now been confirmed in Europe.
As of the end of July, 19 cases of Oropouche fever have been confirmed on the continent, with 12 in Spain, five in Italy and two in Germany, according to the European Centre for Disease Prevention and Control.
Given the relatively high number of travellers between Europe and affected countries such as Brazil or Cuba, Doctor Benjamin Brennan, Senior Research Fellow, MRC-University of Glasgow Centre for Virus Research, predicts we will continue to see sporadic cases of Oropouche fever in returning travellers in Europe.
"We may see cases in the UK in returning travellers that have visited or reside in an epidemic area," he warned.
Health officials are making similar noises across the pond. Florida reported 20 travel-related cases so far this year, including nine last week.
In addition to broadening its geographic spread, the virus appears to be getting more virulent.
In July, health authorities reported the deaths of two adults from the disease — the first since the virus was identified almost 70 years ago.
The deaths occurred in two young Brazilian women who did not have any underlying health conditions.
According to Professor Stephen Graham, School of Biological Sciences Infection and Immunity Theme Leader and Professor of Virus:Host Interactions at the University of Cambridge, this marks "quite a change" in the virus as it has always made people very sick, with debilitating fever and muscle pain for about one to two weeks, and occasionally neuronal symptoms like meningitis, but it has "never before killed people".
Likewise, the age of the two Brazilian women - both in their thirties - is raising alarm bells.
As Assistant Professor Brian Labu of the University of Nevada explains to GB News, young people tend to fight off infection better than their elders so this is a concerning development.
Additionally, Brazilian officials are currently investigating cases of foetal deaths and malformations that might have been caused by the virus, which has now been shown to spread from a pregnant person to their fetus.
"This has potential public health implications so we need to maintain vigilance and monitor the situation carefully," warned Professor Graham.
The third related factor that's making virologists nervous is the route of transmission.
As of yet, there's no hard evidence of human-to-human transmission.
However, the Pan-American Health Organization published a report in July highlighting concerns over possible mother-to-child transmission of the virus.
In one case, a pregnant woman had symptoms of Oropouche and, weeks later, foetal death was confirmed.
The Oropouche genome was detected in several organs of the foetus. In another recent case, a pregnant woman tested positive for Oropouche. The baby was born but died days later. Post-mortem examination identified the virus genome in various tissues, including the brain.
Midges are also an effective vector. Unlike dengue fever, which is spread through the bite of infected mosquitos, midges are very small and can pass through nets and they might be less affected by commonly used insect repellents.
However, some chemical insecticides have proven effective at killing two species of midges.
LATEST HEALTH DEVELOPMENTS

Midges are very small and can pass through nets
|Getty Images
What's driving the current outbreak?
According to Professor Labus, increased dissemination, as with other vector-borne diseases, is driven by climate change, human and animal mobility and behaviour, deforestation, and land use.
Brazil in particular is home to a lot of deforestation. Changing the environment where insect vectors live puts different human and animal populations at risk.
For example, deforested areas are both warmer and drier than similar pristine forests, and studies of Anopheles gambiae, which transmits malaria, have shown that increased larval heat tolerance may have allowed this species of mosquito to widen its range beyond tropical rainforests around the same time early humans were converting central African rainforests into savannah.
Since humans tend to be more concentrated in these areas, those species that prefer humans may experience selective pressure to adapt to the ecological changes.
Urbanisation also creates favourable breeding sites.
There are already signs that this is happening in the ongoing outbreak - Oropouche fever has infected people living in regions far from forested areas for the first time, thus indicating that an urban cycle can exist as well.
Logging in the Amazon and other agricultural developments could also be increasing transmission.
Studies have linked Oropouche outbreaks to increased agricultural activities, highway and road development and bridge construction in South America.
"These activities disrupt ecosystems by causing population migration, vegetation loss (such as deforestation and illegal mining) and changes in agricultural practices. These changes can alter the distribution of wild animal reservoirs and vectors," warned Doctor Enny Paixao, Associate Professor, London School of Hygiene & Tropical Medicine.
Even if the current outbreak stays isolated to rural areas, it could still increase the risk of human-to-human transmission, as people amassing close to the Amazon will increase the likelihood of the virus jumping from wild animals to human hosts, virologists warn.
The other concern stems from the virus's genetic makeup. Oropouche has an RNA genome like SARS-CoV-2 - the virus that causes Covid-19.
RNA, or ribonucleic acid, is a nucleic acid that's present in all living cells and has structural similarities to DNA.
RNA genomes encode proteins that replicate the viral genome and protect it as the virus moves to a new host cell.
Once it gains access to a host cell, it generates abundant copies of its genome, and, through packaging these copies, a virus continues to infect new hosts.
This essentially means that the Oropouche virus is "capable of rapid mutation", warns Professor Graham.
There's evidence that this is happening. A recent study indicated that the main Oropouche virus circulating in the region exhibits significantly higher replication in mammalian cells compared to older strains.
While it remains unclear if this increased replication leads to greater transmissibility by its vectors, it could help explain the recent rise in cases.
As Professor Graham explains, the virus also has a genome with multiple segments, like influenza.
This means that if you are unlucky enough to be infected with two different strains of the virus they can switch their genome segments - a process the virologist likens to "shuffling two decks of cards together" - you might end up with a new virus strain that is more transmissible and more pathogenic.
This process, known as "gene swapping", is how influenza pandemics have started - by swapping genes back and forth, you leapfrog many steps in the adaptation to humans.
There are signs that this reassortment is driving the current outbreak in Brazil.
However, it’s important to note that individual humans or animals being infected by two different strains at the same time is a very rare event, notes Professor Graham.
The most "likely scenario" is that the co-infection and reassortment occurred in a wild animal (sloth, monkey or other), probably some years ago, and was then subsequently transmitted to a human via a biting insect, he says.

Logging in the Amazon and other agricultural developments could also be increasing transmission
|Getty Images
What happens next?
Professor Labu predicts that crucial gaps in knowledge and unrestricted travel to infected areas will continue to drive up cases.
Since it looks like so many other common diseases, doctors are probably not testing for it, so it's likely spreading unchecked, he adds.
Likewise, reported figures are based on laboratory-confirmed cases and taking into account that some individuals will not experience symptoms or seek health care, it’s likely that the true number of infections is higher, warns Doctor Paixao, of the London School of Hygiene & Tropical Medicine.
What should I do if I get it?
In the absence of vaccines or specific treatments, the best advice is to self-isolate and ride it out if you contract the virus, Professor Labu says.
This isn't bad advice since the virus generally results in mild illness.
Virologists also hope the virus will confer natural immunity if it spreads more widely.
If you develop symptoms overseas, TravelHealthPro advises seeking advice from a health professional.
Don't panic...yet
The "good news" is that most people recover completely from Oropouche virus infection within a few weeks, so this virus won’t cause a Covid-like global pandemic, says Professor Graham.
Virologists also agree that ramped-up surveillance could be distorting the numbers.
It's plausible that the increased number of cases and enhanced surveillance are bringing rare events, including deaths, to light.
The same principle applies to the potentially harmful effects on unborn children.
Meanwhile, the European Centre for Disease Prevention and Control has said that there is no evidence that the insects we have in the UK or mainland Europe are capable of transmitting Oropouche virus, so the risk to the general population is low.
The European cases have also been isolated so the risk of subsequent onward transmission is unlikely.
There's also no evidence of secondary transmission of the virus outside endemic areas.
Governments should still update their travel advice to limit exposure to the virus and recommend those heading to infected regions take precautions.
Doctor Philip Veal, Travel Health Consultant at the UK Health Security Agency (UKHSA), said: “When travelling to affected areas, you can avoid the infection, and others such as dengue, Zika and malaria, by preventing insect bites. Use insect repellent, cover exposed skin and sleep under a treated bed net."
Travel Health Pro advised: "If you are planning to visit countries reporting arboviral infections including Oropouche virus, get travel health advice from your GP, practice nurse or a travel clinic, ideally at least four to six weeks before you travel.
"As other diseases such as Zika and malaria may exist in areas where Oropouche virus disease has been reported, pregnant women should discuss the potential risks of their travel plans with their health care provider."
The UK Foreign Office has also issued the following advice: "Before you travel check that your destination can provide the healthcare you may need and you have appropriate travel insurance for local treatment or unexpected medical evacuation. This is particularly important if you have a health condition or are pregnant.
"At least eight weeks before your trip, check the latest vaccination recommendations for Bolivia and see where to get vaccines and whether you have to pay on the NHS travel vaccinations page.
"See what health risks you’ll face in Bolivia, including Oropouche virus disease."
Do not fall asleep at the wheel
The rapid surge of cases of Oropouche fever in South America underscores the importance of increased awareness and enhanced surveillance for the population living in endemic areas and for travellers.
Virologists agree that investments in genotyping surveillance and research that improve our understanding of Oropouche fever are essential in order to develop control measures and therapeutics that can help us to face this emerging threat to global health.
Although Oropouche virus is not new to Brazil, the factors driving the recent sharp increase — including reported deaths and potential foetal harm — highlight the need for further investigation, says Dr Paixao.
"Until advancements are made in vaccine development or mosquito and midge control, or until natural immunity within the population in Brazil increases, the challenge posed by this neglected tropical disease will persist," she warned.