Mpox outbreak: What is the virus, what are Mpox symptoms and is there a vaccine?
The WHO declared mpox a global health emergency
|Getty
The WHO has declared mpox a global health emergency
Don't Miss
Most Read
What is Mpox?
Mpox, formerly called monkeypox, is a rare viral illness caused by the monkeypox virus, a cousin of the smallpox virus. It is most commonly found in west and central Africa although there has been an increase in cases in UK.
Mpox was first discovered in 1958 in monkeys kept for research in Denmark. The first human case was reported in 1970 of a 9 month old boy in the Democratic Republic of the Congo.
The mpox virus has two main types: Clade I and Clade II.
Clade I - This type of mpox tends to cause more severe illness and has a higher mortality rate, with some outbreaks historically leading to deaths in up to 10% of cases. It is predominantly found in Central Africa.
Clade II - The strain responsible for the global outbreak starting in 2022, Clade II generally results in less severe symptoms. Over 99.9 per cent of those infected recover. This clade is mainly found in West Africa.
Mpox symptoms
Mpox symptoms usually appear within 5-21 days, Mpox usually starts with flu-like symptoms such as fever, headache, muscle aches, and swollen lymph nodes.
Within a few days, a rash appears, often beginning on the face and spreading to other parts of the body.
This rash evolves from flat spots to fluid-filled blisters, which eventually scab over and fall off.
The rash can be painful and itchy and might be mistaken for other conditions like chickenpox.
 The WHO declared mpox a global health emergency | Getty
The WHO declared mpox a global health emergency | GettyHow Mpox Spreads
Mpox can spread in various ways:
From Person to Person: Through close physical contact with someone who has the virus, including touching their skin, kissing, or sexual activity. It can also spread through respiratory droplets if you are close to someone who is sick.
From Animals to Humans: By handling or eating meat from infected animals, especially in areas where the virus is common such as west and central Africa.
Through Contaminated Objects: Touching items such as bedding or towels that have been used by someone with mpox can also spread the virus.

Mpox can spread in many ways
| ReutersWhen did the current outbreak start?
A significant outbreak began in 2022 in the Democratic Republic of Congo.
A new viral strain, which first emerged in September 2023, has now been detected for the first time outside the DRC and has rapidly spread to 12 countries in Africa.
On Wednesday, August 14, 2024, the World Health Organisation declared the escalating mpox outbreak an international health emergency and called for vaccine manufacturers to submit dossiers for emergency valuation.
The decision to declare a Public Health Emergency of International Concern (PHEIC) is driven by the emergence of the more deadly strain, Clade 1, which has historically caused fatality rates as high as 10 per cent in previous outbreaks.
Unlike the milder Clade 2, which caused a global mpox emergency in 2022 but was eventually controlled through targeted vaccination, Clade 1 presents a far greater threat.
Recent mutations have led to an offshoot of the virus, Clade 1b, which has been spreading rapidly since September last year. Labelled “the most dangerous yet” by scientists, this variant has already triggered significant outbreaks in regions where mpox was previously non-existent.
"The emergence of a new clade of mpox, its rapid spread in eastern DRC, and the reporting of cases in several neighbouring ring countries are very worrying," WHO Director-General Dr. Tedros Adhanom Ghebreyesu warned.
"On top of outbreaks of other mpox clades in DRC and other countries in Africa, it’s clear that a coordinated international response is needed to stop these outbreaks and save lives.”
What is the WHO saying?
The WHO has outlined an immediate funding requirement of $15 million to support surveillance, preparedness, and response activities. To kick-start these efforts, WHO has already released $1.45 million from its Contingency Fund for Emergencies, with the possibility of more funds being released in the coming days.
WHO Regional Director for Africa Dr. Matshidiso Moeti emphasised the importance of collaborative efforts to curb the virus.
She said: "Significant efforts are already underway in close collaboration with communities and governments, with our country teams working on the frontlines to help reinforce measures to curb mpox.
"With the growing spread of the virus, we’re scaling up further through coordinated international action to support countries bring the outbreaks to an end.”
Current Situation in the UK
While mpox cases have increased in the UK recently, the overall risk remains low.
Most people are unlikely to contract the virus unless they have been in close contact with someone who has it or have travelled to affected areas.
Whilst anyone can get mpox most cases, however, have been in men who are gay or bisexual.
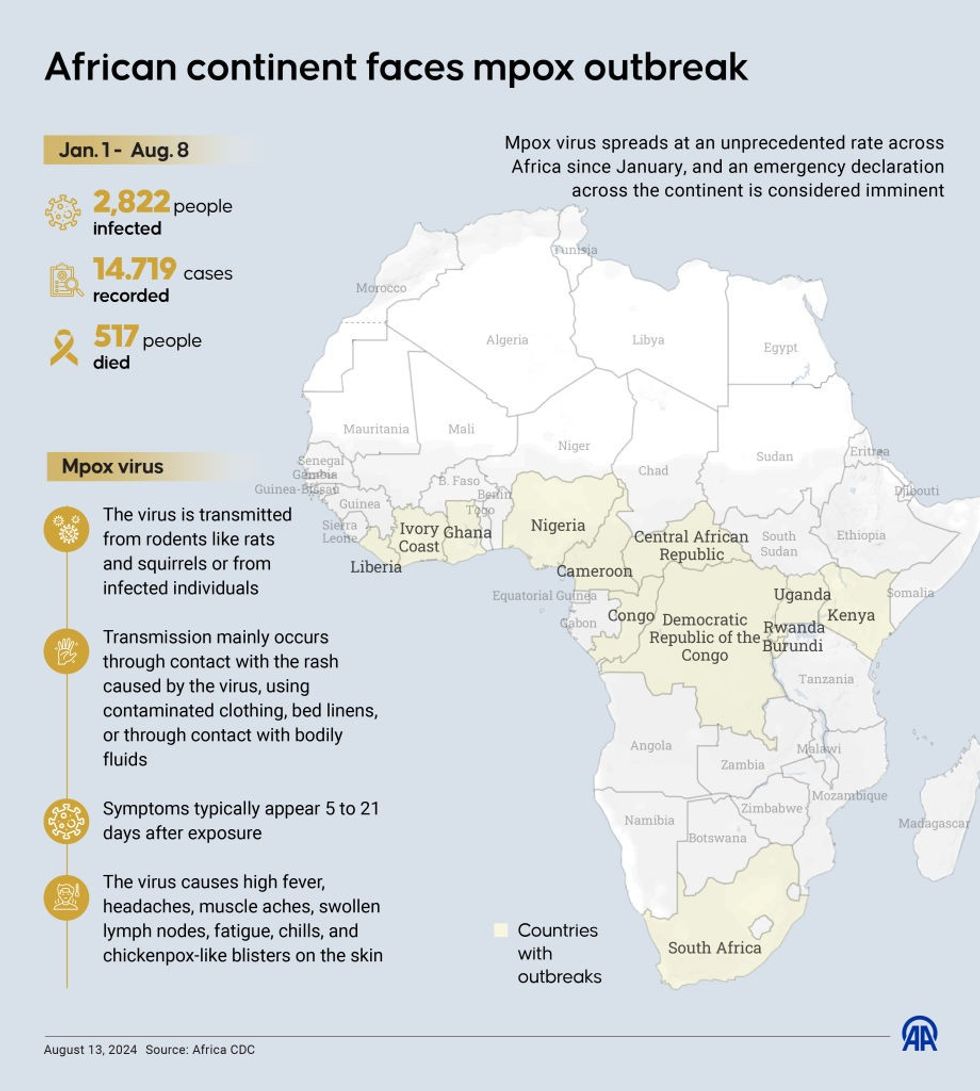
A map of the mpox outbreak in Africa
| GettyWhat to Do if You Have Mpox
If you suspect you have mpox, it is important to:
Seek Medical Advice: Contact a sexual health clinic or your GP if you have symptoms and have been in close contact with someone who might have mpox.
Isolate Yourself: Stay home and avoid close contact with others until your symptoms have completely resolved.
Cover Up: Keep lesions covered and wear a mask around others to prevent spreading the virus.
Recovery
Mpox is usually mild with most people recovering without treatment in 14 to 28 days.
 Zawadi Bwira Bakulu, 35, shows the rash marks on her son Christevie Lukeka who recovered from Mpox in Nyiragongo territory near Goma | Reuters
Zawadi Bwira Bakulu, 35, shows the rash marks on her son Christevie Lukeka who recovered from Mpox in Nyiragongo territory near Goma | ReutersPrevention and Vaccination
Whilst mpox is currently rare in UK, your risk of getting it can be reduced by washing your hands regularly with soap and water or an alcohol based sanitiser, be aware of the symptoms and talk to your partner about their sexual health.
The best way to prevent mpox is to avoid close contact with infected individuals.
The smallpox vaccine, which also protects against mpox, is available for high-risk groups like healthcare workers and people with multiple sexual partners.
If you have been exposed to mpox, getting vaccinated ideally within 4 days can help prevent infection.
The vaccine can be given up to 14 days after exposure to mpox.
In response to the outbreak, WHO is advocating for the Emergency Use Listing of mpox vaccines, a move that would accelerate access to vaccines in lower-income countries.
The two smallpox vaccines currently in use are recommended by WHO’s Strategic Advisory Group of Experts on Immunisation and are approved by national regulatory authorities in several countries, including Nigeria and the DRC.