A deadly new strain of mpox is spreading like wildfire in Central and Western Africa
Getty Images
The spread and severity of Clade 1b has virologists everywhere worried - but how worried? Our Health Editor investigates
Don't Miss
Most Read
Trending on GB News
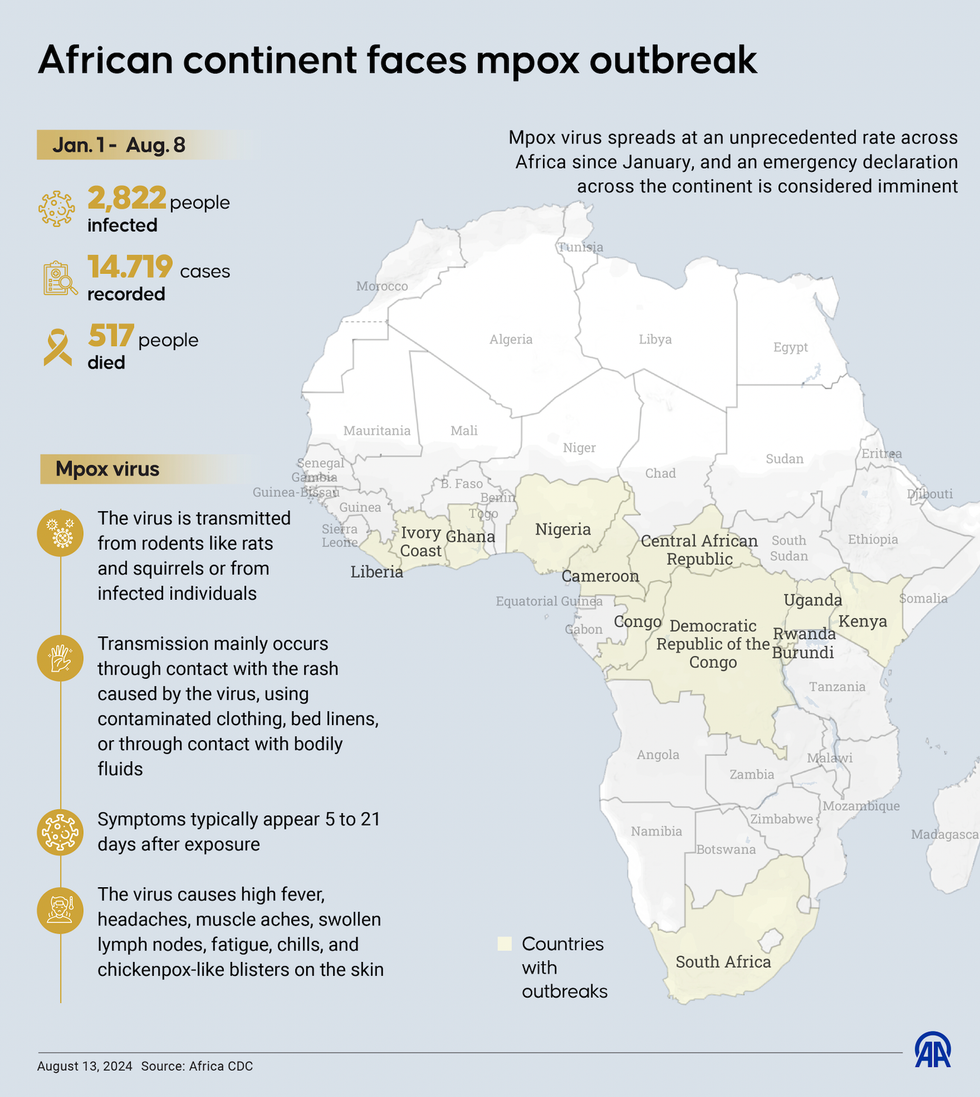
Mpox is a viral disease that causes fluid-filled skin lesions, fever, flu-like symptoms and in severe cases, death.
The disease, formerly known as monkeypox, has been circulating in humans and wild animals in Central and West Africa for decades.
It was first detected in humans in the Democratic Republic of the Congo in 1970.
Mpox is spread between people, mainly through close contact, and occasionally from the environment to people via things and surfaces that a person with mpox has touched.
It is also zoonotic, meaning it can jump from animals to humans.
There are two distinct lineages of mpox: Clade 1 and Clade 2.
In 2022, a subtype of Clade 2 rapidly spread around the globe, turning up everywhere from Australia to America. It also spread across Europe for the first time.
At the time, the World Health Organization (WHO) declared the outbreak to be a public health emergency of international concern but cases were mild and confined to men having sex with men. WHO subsequently lifted the global health emergency in May 2023 after cases declined.
In April of this year, researchers who analysed samples collected in the DRC province of South Kivu in late 2023 and early 2024 revealed that they had identified a subtype of Clade 1, called Clade 1b.
Cases have surged in the DRC, infecting nearly 8,000 people in 2024 alone.
Getty Images
They determined it spreads effectively between people through various means including sexual contact.
It originated among sex workers in the mining town of Kamituga, around 170 miles (273km) from the border with Rwanda, in September of last year.
There have been more than 14,000 cases and 511 deaths recorded in the DRC this year alone.
A significant number of these cases have been among children - 40 per cent of cases are in children under five years old.
Cases have now been confirmed in four neighbouring countries that have not reported mpox previously: Burundi, Kenya, Rwanda and Uganda.
It's thought the majority of these cases are caused by Clade 1b.
This prompted the World Health Organization (WHO) to declare a global health emergency on August 14.
A day later, Swedish health officials announced that there had been one confirmed case of Clade 1b in Stockholm.
It is understood that they had been infected during a visit to Africa. This is the first known imported case of Clade 1b in Europe.
The UK Health Security Agency (UKHSA) said there are currently no cases in the UK and the risk to the population is low.
However, it was on alert for any cases of the virus.
Why all this is worrying
There are several reasons to be concerned about the spread of Clade 1b.
Take transmission first. Unlike Clade 2, which was confined to men having sex with men, Clade 1b is "bleeding out" to the wider community, spreading through heterosexual contact, pregnant women and children, warns Assistant Professor Brian Labu of the University of Nevada in Las Vegas.
The public may not be cognizant of this, which could breed complacency.
The professor likens this insouciance to the aids epidemic in the 80s, where it was "mostly men who had sex with other men but not exclusively", he says.
By 2020, 49 per cent of new HIV diagnoses were in heterosexuals compared to 45 per cent in gay and bisexual men, according to figures from the UKHSA.
It's conceivable that mpox could go this same way if steps are not taken to contain its spread among the wider population.
Where it's spreading is also worrying, according to Doctor Brian Ferguson, Associate Professor of Immunology at the University of Cambridge,
This takes us back to Africa. As Doctor Ferguson points out, the current outbreak is taking place in a region where HIV prevalence is relatively high but access to antiretroviral drugs is poor.
"There is further concern about the lack of access to vaccines and a globally slow response to vaccine production and distribution," he said.
Even though there are existing effective vaccines, there are not enough doses and they are not being getting to where they are needed, the professor warns.
LATEST HEALTH DEVELOPMENTS

Even though there are existing effective vaccines, there are not enough doses
Getty Images
Professor Labu shares his concern, adding that the biggest challenge to containing Clade 1b is the "low-income environment" in which it's spreading.
Poor populations in Central and Western Africa do not have the same access to testing or vaccination, he laments.
Or as Professor Jimmy Whitworth, Emeritus professor London School of Hygiene and Tropical Medicine, put it: "The epicentre of the epidemic in South Kivu is undergoing a protracted humanitarian crisis and getting the necessary facilities in place for surveillance, diagnostic testing, contact tracing and case management, is going to be very challenging."
The amount of vaccine required has been estimated by Africa CDC to be 10 million doses.
The cost and availability of vaccination is one thing but shoring up global solidarity to ensure rich countries, such as America or the UK, do not stockpile vaccines is another.
Figuring out these logistics matters because Clade 1b is more transmissible and deadlier than Clade 2.
In the 2022 outbreak, fewer than one per cent of people died.
Clade 1b appears to have a death rate of about three to four per cent.
According to the Africa Centers for Disease Control and Prevention, 96 percent of all cases and deaths in the region are in Congo.
Cases are up 160 per cent and deaths are up 19 per cent compared with the same period last year. So far, there have been more than 14,000 cases and 524 people have died.
Officials at the Africa CDC said nearly 70 per cent of cases are in children younger than 15, who also accounted for 85 per cent of deaths.
The time to act is now
According to Doctor Eoghan De Barra, Consultant in Infectious Diseases, Beaumont Hospital, and Senior Lecturer, RCSI University of Medicine and Health Sciences, the moves by the WHO should focus the research and medical communities and signal to governments that they should assess their planning and preparedness.
The first case in Sweden should serve as a wake-up call too.
"We have the tools to limit the impact of mpox on human health, but need resources, education and ongoing scientific investigation to optimise them," Doctor De Barra said.
According to Doctor Connor Bamford, Lecturer, School of Biological Sciences at Queen’s University Belfast, this will require efforts in Africa as well as globally, which should involve sharing crucial life-saving vaccines with the affected African nations and seeking to eliminate the spread in other regions through robust surveillance measures.
Diagnostic PCR tests can differentiate between Clade 1 and Clade 2 based on genetic differences between these two strains.
So far, sequencing of the virus genome has been used to confirm Clade 1b cases in Africa.
The availability of these new Clade 1b genomes will allow the development of diagnostic PCR tests to differentiate between Clade 1 and Clade 1b as well.
The UK is preparing for any potential cases by ensuring clinicians are aware of mpox and able to recognise cases promptly.
Rapid testing is also being made available, while protocols are being developed for the safe care of potential patients to prevent transmission.
These surveillance efforts are critical because to better understand the mortality rate we need to better understand the number who are infected overall, including those with milder disease and how they are infected, explains Professor Trudie Lang, Professor of Global Health Research and Director of The Global Health Network, University of Oxford.
"We need to also understand better the relationship between transmission route and severity of disease," she continued, adding: "This disease impacts highly vulnerable communities and there is already much stigma associated with this. Therefore, we need to understand people’s perceptions and practices to enable effective public health interventions and messages to encourage treatment seeking and guide safer practices to reduce risk of infection."
As she rightly points out, this will be crucial for vaccine uptake: "Vaccines are imperative and existing ones, as well as those in development, need to be tested in the regions where Clade 1b is escalating to assess if they work in this variant and to get traction in preventing further spread to further new regions both in Africa and globally."
This means improving on past efforts. Western countries during the 2022 outbreak mostly shut down the spread of mpox with the help of vaccines and treatments, but very few of those have been available in Africa.
Africa CDC said last week it had been granted £8.1million in emergency funding from the Africa Union for its mpox response, and its director general Jean Kaseya said on Tuesday there was a clear plan to secure three million doses of vaccine this year, without elaborating further.
Meanwhile, the share prices of several healthcare and pharmaceutical companies jumped last week following WHO's emergency declaration as speculation grew over the need for mass vaccination programmes.
Congo will receive the first vaccine doses to address its mpox outbreak next week from the United States, the country's health minister said on Monday.








