Britons furious after new drug found to slow Alzheimer's for the first time is BLOCKED on NHS: 'Disgraceful!'
Britons have blasted the decision to block lecanemab on the NHS, dubbing it another sign of broken Britain
|Getty Images

Health regulators deemed lecanemab too costly to justify
Don't Miss
Most Read
Britons are raging after UK regulators blocked the use of a breakthrough Alzheimer's drug on the NHS.
The National Institute for Health and Care Excellence (Nice) said the benefits of lecanemab, which is approved for UK use, are too small to justify the significant cost to the NHS.
Meanwhile, the Medicines and Healthcare products Regulatory Agency (MHRA), who granted the licence, said it is efficient at slowing Alzheimer’s disease.
The medical community may be divided but public opinion isn't, with netizens raging at what they view as another sign of broken Britain.
Taking to X, one user branded the decision "absolutely disgraceful", while another called it "two-tier healthcare" in action, claiming that it "indicates that the lives of Alzheimer's sufferers in the UK are not worthy".
A third person pointed to the terrible optics, which signal that "greed and profits are way more important".

The Medicines and Healthcare products Regulatory Agency (MHRA) said it is efficient at slowing Alzheimer’s disease
|Getty Images
Do they have a point?
The reality is more complicated than netizens are making out.
As Professor Paul Morgan, Interim Director, UK Dementia Research Institute Cardiff, Cardiff University, explains, the U.S. Food and Drug Administration (FDA) decision and subsequent MHRA approval was based on the trial evidence showing a modest decrease in rate of progression in mild cognitive impairment (MCI) and early Alzheimer's patients treated with lecanemab for up to two years.
NICE reassessed this evidence and undertook a cost-benefit analysis, concluding that the socioeconomic case for using lecanemab, which costs about £20,000 per patient per year in the US, was not made.
“Even in the company analysis of the first large trial results, the impact of the drug was relatively small, claiming a 27 per cent slowing of cognitive decline; others have suggested that, when dropouts and other cofounders are taken into account, the impact may be substantially smaller," he explained.
According to the professor, the NICE guidance does not specifically address risks of the drug – which are significant.
As many as a quarter of treated individuals can develop signs of a brain vascular injury termed ARIA, mild in most but can be severe and occasionally fatal in a small number of people.
"There have been several deaths from this condition in the US and there is considerable effort to identify and exclude those most at risk, including individuals homozygous for the Alzheimer risk gene ApoE4 and those with preexisting brain vascular problems," he explained.
He continued: “The anti-amyloid drugs emerged with considerable media hype, unsurprising considering that these were the first to show ANY disease-modifying effect in AD. The combination of high cost of the drug, relatively low impact on disease and significant risk likely justify the NICE guidance. It is possible that, as better ways of identifying those most likely to benefit emerge and the result of longer-term use in the US are revealed, the balance may shift and the guidance change.
“The NICE decision is likely to be disappointing to those affected by AD whose hopes may have been elevated by the early promise of amyloid-targeting therapies; however, given the many unanswered questions around patient selection, monitoring, long-term impact and side effects, the “wait and see” approach is understandable.”
Others disagree with this assessment, with Professor Bart De Strooper, Professor in Alzheimer’s Disease at UCL and UKDRI branding the decision "disappointing", adding: "NICE and the UK have not seized this opportunity to send a clear signal to NHS that the future for Alzheimer’s Disease is starting and that they better prepare for it. We should start now to improve the diagnosis and support systems for Alzheimer’s patients. While better drugs are on the horizon, it would have been more forward-thinking to see this drug as an opportunity to begin strengthening the support infrastructure now, in preparation for a future where dementia can be effectively managed or even eradicated.
The prof continued: "It's also unfortunate that those who could benefit from this treatment but cannot afford it will be left without access. The data and the rumours at the international Alzheimer’s Congress suggest that some patients are very much helped with this treatment. We will learn from the countries who fully support the use of the medication.”
LATEST HEALTH DEVELOPMENTS

The company analysis even concluded the impact of the drug was relatively small
|Getty Images
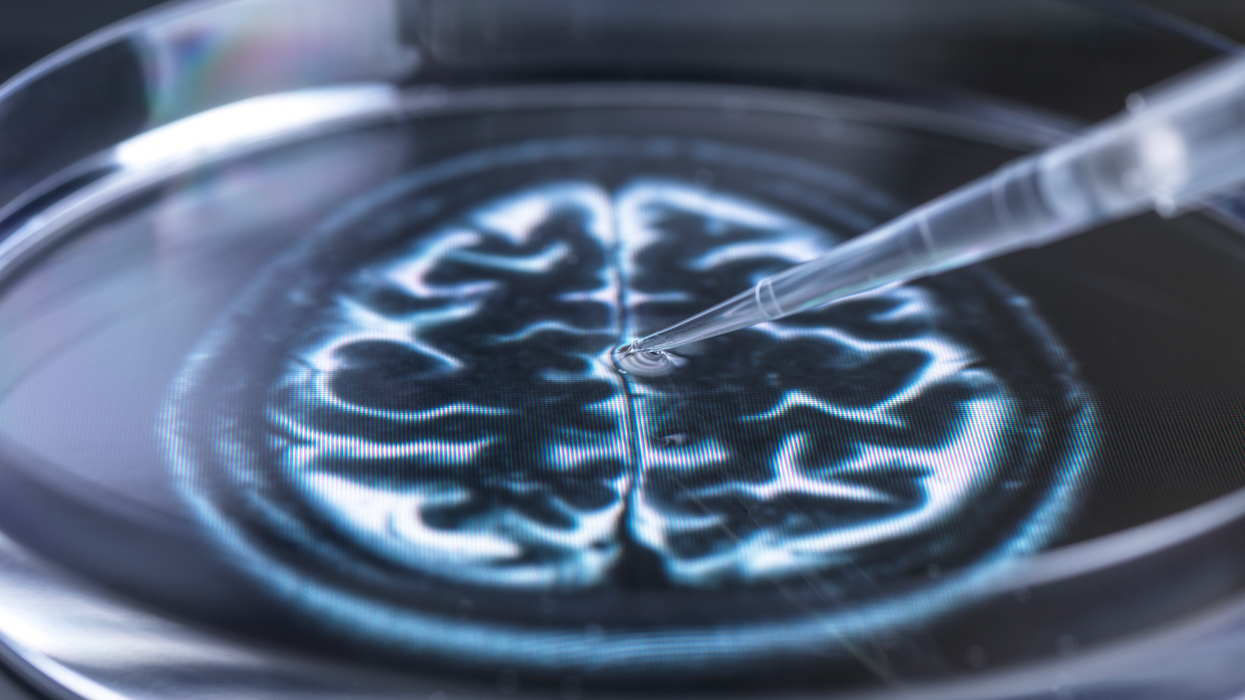
How does it work?
Lecanemab is an antibody drug that has been shown to slow down the early stages of Alzheimer’s.
It works by binding to a protein known as amyloid, which builds up in the brains of people living with the disease.
The drug has been developed by Eisai, a Japanese pharmaceutical company, and is sold under the brand name Leqembi.
Lecanemab been shown to successfully remove amyloid build-up from the brains of people living with early Alzheimer’s disease.
For people taking the drug, 18 month-long trials showed the decline in thinking and memory skills slowed down by 27 per cent.
It also slowed down the decline in quality of life by up to 56 per cent.
These trial results were hailed by experts as a milestone as it was the first time a drug had shown the underlying mechanism of the disease could be slowed.