Respiratory illnesses are soaring four years on from the start of the Covid pandemic
Getty Images
The Covid pandemic is in the rearview mirror but a disturbing trend is emerging. Our digital health editor investigates
Don't Miss
Most Read
Trending on GB News
Marie thought she had contracted the flu when she went to her GP.
Her symptoms had been getting progressively worse since January but she was toughing it out.
"I had the most awful night sweats and noticed that I had lost a fair bit of weight," the 42-year-old told GB News.
After spotting a shadow on her lung, the doctor told Marie she had tuberculosis.
"I was immediately admitted to hospital and put into isolation. I don’t think I realised how ill I was until I was admitted."
The mother from Belfast had a torturous road to recovery. At her lowest point she had dropped to four stone and was "weary with a racking cough".
Days would go by where she "could barely stand and walk. The night sweats, the cough, the back and lung pain were all horrendous and I felt like my body was just wasting away".
Marie is no outlier. TB is on the rise across much of the world.
Cases jumped by more than 10 percent last year in England alone - a trend that has continued into 2024, UK Health Security Agency (UKHSA) data shows.
Other respiratory illnesses are also making a comeback. Elevated influenza activity was reported in countries in Central America, the Caribbean and South Asia in the week ending 2 June 2024, the latest World Health
Organization shows.
In the Southern Hemisphere, countries in South America, South Africa, and Oceania reported elevated influenza activity.
Rates of whooping cough, polio, dengue and cholera are also surging worldwide, a new analysis by Airfinity and Bloomberg News reveals.
It is not lost on researchers that rates of infection are skyrocketing in the wake of the Covid-19 pandemic.
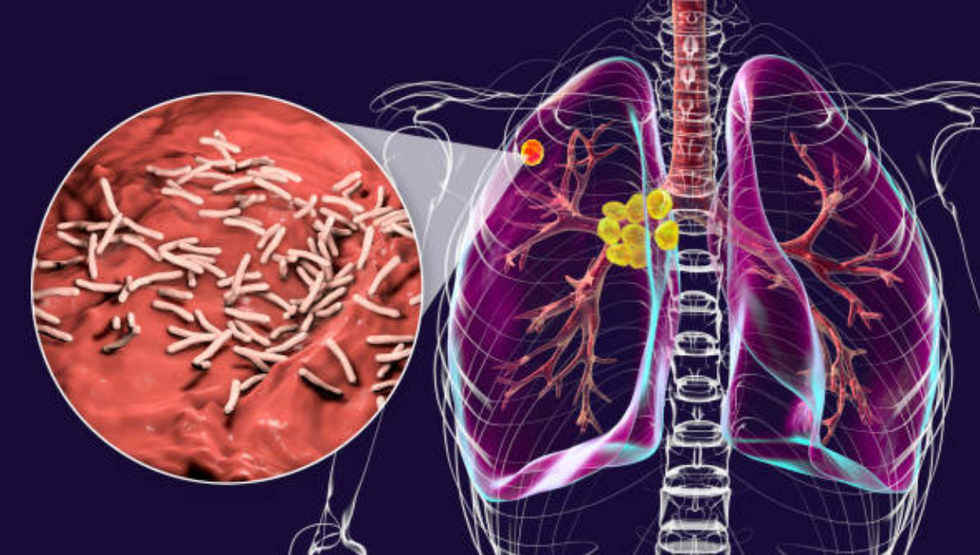
Cases of TB jumped by more than 10 percent last year in England - a trend that has continued into 2024
Getty Images
The surge in various illnesses in the aftermath of COVID-19 presents a "complex interplay of immunological, societal, and healthcare-related factors that merit a detailed examination", Veronika Matutyte, a medical doctor at the Lithuanian University of Health Sciences, tells GB News.
There's increasing evidence that SARS-CoV-2 - the virus responsible for COVID-19 - can cause lasting alterations in the immune system.
Doctor Gareth Nye, Programme lead for Medical Science at the University of Chester, finds the evidence compelling.
"The Covid virus has been proven to show structural changes to the respiratory system which may make you more prone to respiratory disease and illness, particularly in the 24 months after contracting the disease," he told GB News.
A study published in the journal Lancet looked at the risks of respiratory diseases following Covid infection.
Researchers crunched data from the UK Biobank database on hundreds of thousands patients and concluded that patients infected with Covid "exhibited elevated risks" for developing respiratory diseases.
Possible explanations include Covid-19 persisting in tissues (including the respiratory tract) as well as the circulating system for an extended period of time after the initial infection.
This prolonged presence of the virus may have directly contributed to long-term damage of the respiratory tissues, consequently leading to the development of various respiratory diseases, researchers posit.
Second, it has been observed that Covid infection can lead to prolonged immunological dysfunctions, including highly activated innate immune cells and increased expression of pro-inflammatory cytokines.
These immune system abnormalities are closely associated with common chronic respiratory diseases.
How much all this accounts for the rebound in respiratory illnesses is hard to say, although some researchers think the effect is exaggerated.
For example, several studies have now shown that, in response to SARS-CoV-2, specialised white blood cells called lymphocytes grow in number.
These lymphocytes also display changes in their features typical of cell activation, such as changes in surface proteins - a key factor in infection.
Such changes may sound menacing but they’re normal and merely indicate that the immune system is working as it should.
For most people, the immune system appears to regain balance following recovery.
However, a subset of patients go on to develop long Covid and research has found these patients display signs of immune dysfunction and exhaustion. This could in theory leave them more vulnerable to infection from other respiratory illnesses.
Unfortunately, the medical profession cannot even agree on a definition for long Covid, let alone determine its impact on the body's ability to fend off other infections.
But it is worth looking into: recent ONS data shows that in the first four months of this year, the number of people in England and Scotland with long Covid increased by 9.9 percent to two million. That's approximately one in every 32 people.
LATEST DEVELOPMENTS
- New test predicts Parkinson's years before symptoms appear
- Cancer in young people is on the rise - why?
- Daily use of Listerine may increases the risk of cancer
Opening Pandora's box
The surge in respiratory illnesses is also being attributed to the lockdown measures imposed during the pandemic.
One theory that has gained traction is that social isolation weakened "herd immunity" - the controversial idea that a significant portion of a population becomes immune to an infectious disease once it is sufficiently exposed to it either through vaccination or natural infection.
When children are compromised, the lack of immunity influences others as well, the theory goes.

Long Covid patients display signs of immune dysfunction and exhaustion
Getty Images
This might explain the surge in whooping cough cases in the UK since the pandemic, which has resulted in the death of eight infants this year alone.
The notion that immunity debt - the idea that immune systems become weaker through a lack of disease exposure -caused a surge in respiratory illnesses, appears to have originated from a position paper published in August 2021 in the journal Infectious Diseases.
French researchers suggested many infectious diseases like RSV that receded during the pandemic quickly rebounded once people stopped masking and isolating themselves.
The researchers argued that a lack of exposure to infectious diseases during lockdowns left us with compromised immune systems.
In their concluding remarks, they concede that their idea is merely a hypothesis, not a fact backed up by rigorous scientific evidence.
Indeed, the immunological argument is far from settled.
For example, it doesn't necessarily follow that we require a constant background of infection for our immune system to function properly. But a simple case can be made without drilling down into the science.
Take influenza. Social distancing measures significantly reduced influenza rates initially.
As normal interactions have resumed, the population's exposure to such pathogens has increased without the usual seasonal preparation, leading to sharper spikes in disease incidence.
This 'triple burden' of flu, RSV and COVID-19 is placing considerable strain on the NHS each winter.
Or, as Doctor Matutyte of the Lithuanian University of Health Sciences puts it, the "backlog" of healthcare services has created a scenario where preventable diseases have gained a "foothold".

The population's exposure to pathogens has increased without the usual seasonal preparation since the pandemic
Getty Images
Tried and tested
The most provable hypothesis is that opening up again has led to a frenzy of testing which has sent recorded rates soaring.
The COVID-19 pandemic had a "devastating effect" on TB surveillance in particular, notes Doctor David Schwartz, a medical epidemiologist based in the US.
This included decreased screening and delayed or missed diagnoses of new TB cases, the doctor laments.
Indeed, TB health programs were "stretched thin" during and after the pandemic, Teresa Austin Karre of the College of American Pathologists, tells GB News.
The reported number of people newly diagnosed with TB fell from 7.1 million in 2019 to 5.8 million in 2020. There was a partial recovery to 6.4 million in 2021, but this was still well below pre-pandemic levels.
Likewise, total influenza cases in the US last season were 28 percent higher than in 2019. In Europe, total influenza cases last season were 75 percent higher than in 2019.
The world might therefore be playing catch up.
Sleeves down
The other possible cause is low vaccination rates.
Disruptions caused by the COVID-19 pandemic have contributed to a decline in vaccination uptake and an increased incidence of several infectious diseases.
This helps explain the resurgence of diseases like measles, whooping cough, polio and RSV in children.
It also underscores the importance of getting vaccinated. Research consistently shows that vaccination blunted the worst effects of Covid and the same can be said for other respiratory illnesses.
However, the Covid pandemic accelerated a disturbing trend.
As Doctor Vanessa Saliba, consultant epidemiologist at the UKHSA explains, a decline in vaccine uptake over the last decade was “exacerbated” by the Covid-19 pandemic.
This is especially true of polio. Childhood vaccination coverage in England decreased in 2022/23 compared to the previous year, NHS figures show. No vaccines met the 95 percent target during the pandemic.
This trend has many complex causes but one that gets less attention is "vaccine fatigue".
According to Doctor Schwartz, who is also a Fellow of the College of American Pathologists, widespread messaging to enhance distribution of COVID-19 vaccines and boosters since 2021 has resulted in a vaccine fatigue phenomenon which has challenged the implementation of vaccines for other infections.
It doesn't help that vaccine hesitancy was dialed up during the pandemic as people in their droves turned to the dark corners of the internet.
A national survey conducted in England earlier this year reported a rise in the number of parents saying they had come across information that left them concerned about getting their children vaccinated, with the primary sources being the internet and social media.
Some 20 percent of parents were left worried about vaccinations after seeing this content in 2023, up from six percent in 2022.
This appeared to have a real impact: the proportion of children who had received their first MMR jab by the age of five decreased to 92.5 percent – the lowest level since 2010/11 - during those years.
This might be coincidental but it does point to a very real problem that needs addressing: MMR jab protects against 13 diseases, including measles, polio, diphtheria, mumps, whooping cough, rubella and meningococcal infections, which can lead to meningitis.

Disruptions caused by the COVID-19 pandemic have contributed to a decline in vaccination uptake
Getty Images
What can be done about all this?
In the context of escalating incidences of RSV, tuberculosis, and influenza, it is imperative to adopt a "multi-layered approach" to health protection that extends beyond "conventional wisdom", says Joseph Ambani, medical doctor and infectious disease expert.
For Doctor Ambani, this takes the form of personalised and community-wide strategies to effectively combat these threats.
Beyond the standard recommendations for vaccinations, he encourages the consideration of timing and population-specific vaccine strategies
For instance, timing flu vaccinations to ensure peak immunity during the highest-risk months can significantly enhance efficacy.
Additionally, expanding RSV immunisation recommendations to include other high-risk groups, beyond just infants and the elderly, could substantially reduce the burden of disease.
To cut the NHS some slack, it has already implemented many of these strategies while acknowledging that there is much more work to be done.
Last year Steve Russell, Chief Delivery Officer and National Director for Vaccinations and Screening for NHS England, published his vaccination strategy which he says "brings together all vaccination programmes, for the first time, to protect communities and save lives".The vaccination strategy includes:
- Improving access including an expansion of online services: The ‘front door’ to vaccination services should be simple to understand. Many more people will be able to book their vaccines online quickly and easily, including via the NHS App. Families will be able to view their full vaccination record with clear information and guidance on what vaccinations they should have to keep them well
- Vaccination delivery in convenient local places, with targeted outreach to support uptake in underserved populations: It should be easy for people to take up the vaccination offer, with sites at GP practices and pharmacies as well as shopping centres, supermarkets and community centres. Bespoke outreach services should be tailored to communities that are un- or under-vaccinated, building trust and confidence.
- A more joined-up prevention and vaccination offer: Vaccination services and activities should be holistic, offering multiple vaccinations for the whole family where appropriate, including covid and flu alongside, for example, opportunistic MMR and HPV catch-up. Multidisciplinary teams could offer wider health advice and interventions such as blood pressure, diabetes and heart checks, or mental health and dental information.
It is worth highlighting here that the flu vaccine is currently recommended for everyone over six months of age, with particular emphasis on high-risk groups such as young children, the elderly, pregnant women, and individuals with chronic health conditions.
The best way to prevent polio is to make sure you and your child are up to date with your vaccinations.
 A Phase 3 clinical trial is currently underway to assess the efficacy of a potential new TB vaccineReuters
A Phase 3 clinical trial is currently underway to assess the efficacy of a potential new TB vaccineReutersGreater investment in vaccine research is still needed to widen the pool of potential candidates.
The only available TB vaccine, for example, dates back to 1921. BCG protects babies and young children against severe forms of TB, but it offers inadequate protection for adolescents and adults against the pulmonary form of the disease, which is primarily responsible for the transmission of the TB bacterium.
There are reasons to be optimistic. A Phase 3 clinical trial is currently underway to assess the efficacy of a potential new TB vaccine, with first doses given in South Africa, where TB takes a heavy toll.
As for RSV, while there isn’t a widely available vaccine yet, several candidates are under development and show promise in clinical trials.
Cutting through
Public health messaging in general needs to be improved.
Educating the public about the transmission dynamics of these diseases, and the importance of timely medical consultation for respiratory symptoms, can "empower" individuals to take action early, potentially curtailing the spread of infections, Doctor Ambani tells GB News.
What form might these early interventions take?
The general public needs to clue themselves up on the role of nutrition in reducing the risk of RSV, tuberculosis, influenza, and other infectious diseases and the reliance of the body’s immune responses on certain micronutrients, says Pharmica's Superintendent Pharmacist Carolina Goncalves.
"Certain vitamins such as vitamins A, C, and E are closely linked to the production and optimal functioning of immune cells," she told GB News.
These include:
- Vitamin A - the body converts a compound called beta-carotene (found in high concentrations in carrots, sweet potatoes and spinach) into vitamin A. Research shows that certain vitamin A derivatives such as retinoid acid can bolster the immune system, given the role Retinoid acid plays in the regulation of immune cells and their ability to counter pathogen invasion.
- Vitamin C - commonly found in citrus fruits, vitamin C has been found to stimulate the production and function of white blood cells. According to research, vitamin C enhances the ability of a type of white blood cell called neutrophils to destroy pathogens. Moreover, vitamin C has been shown to improve the function of lymphocytes (cells that help with adaptive immunity), protecting against infectious diseases.
- Vitamin E - Vitamin E occurs in high concentrations in certain types of nuts, such as almonds and sunflower seeds, as well as in leafy vegetables like broccoli. Studies show that vitamin E helps enhance the activation of T cells and may potentially help modulate the production of inflammatory chemicals called cytokines, thereby supporting the immune system in preventing and mitigating infectious diseases.
Hand hygiene is one of the most important ways to prevent infections.
It kills pathogens that can be transmitted through touch. Proper hand-washing methods with soap and water or hand sanitiser eliminate bacteria, viruses, and other microorganisms from the skin.
"It is particularly effective in preventing the spread of respiratory and gastrointestinal infections," noted Goncalves.
A study highlighted that individuals who practised proper hand hygiene had a 21 percent lower risk of contracting respiratory illnesses compared to those who did not.
This emphasises the critical role of hand hygiene in preventing the transmission of respiratory pathogens.
The NHS recommends washing hands thoroughly for at least 20 seconds with soap and water to prevent the contraction and spread of infectious diseases.

Research shows that certain vitamin A derivatives such as retinoid acid can bolster the immune system
Getty Images
Exercise may also help. A study shows the most effective kind of exercise to boost immunity is moderate-intensity aerobic exercise for less than 60 minutes.
This type of exercise increases immune cells such as tissue macrophages and improves the circulation of antibodies, anti-inflammatory molecules, and T-cells, all of which are important for fighting infections and maintaining good health, explains Goncalves.
Other important interventions include:
- Cutting down on alcohol - Research has shown that excessive alcohol intake impairs the body's ability to fight off infections by reducing the efficiency of immune cells and cytokine production.
Getting enough sleep - Research indicates that during sleep, the immune system produces proteins called cytokines, which are crucial in combating infections and inflammation. These cytokines stimulate and mobilise immune cells to affected areas, thereby enhancing the body's ability to heal and defend against pathogens. Adequate sleep increases the production of these protective cytokines and improves the efficiency of immune cells, which strengthens the immune response.
Eyes wide open
Global and local surveillance symptoms also need a major upgrade, although progress is afoot on this front.
In light of the impact of the COVID-19 pandemic, WHO’s 194 Member States established a process to draft and negotiate a new convention, agreement, or other international instrument on pandemic preparedness and response.
This agreement, known as the Intergovernmental Negotiating Body (INB), was driven by the need to ensure communities, governments, and all sectors of society – within countries and globally – are better prepared and protected, in order to prevent and respond to future pandemics. It equally applies to the spread of respiratory diseases.
On 1 June 2024, the World Health Assembly extended the mandate of the INB, deciding that this work on the proposed WHO Pandemic Agreement must be finished as soon as possible.
A key objective is to better link up local surveillance data to global networks.
"This approach ensures that emerging trends in infectious diseases are identified swiftly, allowing for immediate and effective responses," added Doctor Ambani.








