Bird flu pandemic fears soar as scientists discover new route of transmission: 'Impossible to stop'

Scientists are getting nervous after finding a new carrier of bird flu - and could be 'impossible' to stop
|Getty Images

The discovery of a new vector comes as research suggests human cases are going undetected
Don't Miss
Most Read
Scientists are sounding the alarm after discovering a new route of transmission for bird flu.
Virologists were already nervous after avian influenza A (H5N1) jumped to cows for the first time in March.
Since then, avian influenza has been detected in at least 175 dairy farms in 13 states across America - and it is spilling over into humans.
So far, 14 human cases have been linked to the dairy outbreak: four in dairy farm workers and 10 in workers on poultry farms with infections linked to the dairy outbreak. It is feared that many more are going undetected.
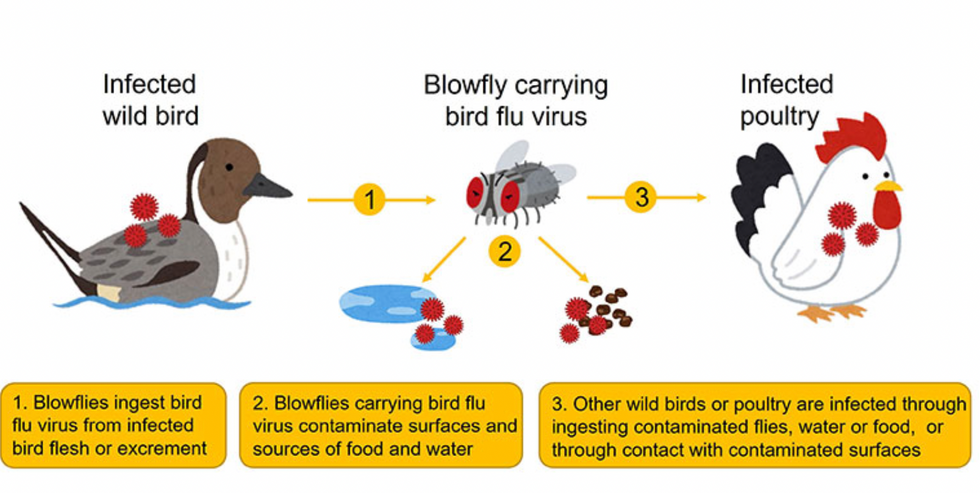
Transmission of bird flu from infected wild birds to other wild birds or poultry via blowflies
|Kyushu University
Now, researchers have identified a new and more cunning carrier in another part of the world.
Researchers from Kyushu University have discovered that blowflies - a family of flies strongly attracted to decaying flesh and faeces - are carrying bird flu in southern Japan.
Their findings, published in Scientific Reports, highlight the need to develop new countermeasures to prevent and control the disease in poultry farms.
It is unclear if this vector poses a greater threat to human-to-human transmission than cows but the signs are not good.
Unlike birds and mammals which the virus infects and replicates inside, blowflies instead ingest the virus from infected dead birds or their waste, with the virus maintaining infectivity for up to two days.
Blowflies are capable of flying at least two kilometres per day, so the researchers estimate that is it feasible for them to reach nearby poultry farms or other wild bird populations within a four-kilometre range.
The researchers believe that as the blowfly moves from place to place, it could contaminate surfaces, food sources and water sources, with healthy birds becoming infected through direct contact with these contaminated sources, or by ingesting adult or larval blowflies.
"By keeping areas clean and using fly control methods, such as fine nets or insecticides, we can reduce the risk of virus spread to indoor poultry farms. However, in outdoor farms in other countries, and in wild bird populations, controlling blowflies may be logistically impossible,” warned first author Associate Professor Ryosuke Fujita of Kyushu University’s Faculty of Agriculture.
LATEST DEVELOPMENTS

So far, 14 human cases have been linked to the dairy outbreak in 13 states
| Getty ImagesFor the study, the researchers collected 648 blowflies and discovered that 14 blowflies were carrying the bird flu virus. The majority of virus-positive blowflies were collected from the sample site closest to the crane colony.
"While 14 blowflies may seem like a low number, this represents a prevalence in blowflies of 2.2 percent, which is a huge percentage compared to other diseases spread by insects,” explained Fujita.
The research team also used genetic testing to confirm that the blowflies were carrying the same virus strain that has been infecting the crane colony.
Meanwhile, a small study in Texas suggests that human bird flu cases are being missed on dairy farms.
The study, which is yet to be peer-reviewed, focused on two undisclosed dairy farms in Texas that experienced H5N1 outbreaks in their herds starting in early and late March, respectively.
The researchers had a previously approved research protocol to study novel respiratory viruses on dairy farms.
"Farm A" had 7,200 cows and 180 workers. Illnesses began on March 6, and nearly 5 per cent of the herd was estimated to be affected during the outbreak. "Farm B" had 8,200 cows and 45 workers. After illnesses began on March 20, an estimated 14 per cent of the herd was affected.
The researchers first visited Farm A on April 3 and Farm B on April 4, collecting swabs and samples at each. Based on the previously approved protocol, they were limited to taking nasal swabs and blood samples from no more than 10 workers per farm. On Farm A, 10 workers provided nasal swabs and blood samples. On Farm B, only seven agreed to give nasal swabs, and four gave blood samples.
While swabs from cows, milk, a dead bird, and a sample of faecal slurry showed signs of H5N1, all of the nasal swabs from the 14 humans were negative. However, when researchers looked for H5N1-targeting antibodies in their blood—an indicator that they were previously infected—two of the 14, about 14 per cent, were positive.
Both of the workers with previous infections, a man and a woman, were from Farm A. And both reported having flu-like symptoms. The man worked inside cattle corals, close to the animals, and he reported having a cough at the time the samples were taken.
The woman, meanwhile, worked in the cafeteria on the farm and reported recently recovering from an illness that included fever, cough, and sore throat. She noted that other people on the farm had similar respiratory illnesses around when she did.
The finding suggests human cases of H5N1 are going undetected. Moreover, managing to find evidence of two undetected infections in a sample of just 14 workers suggests it may not be hard to find more.