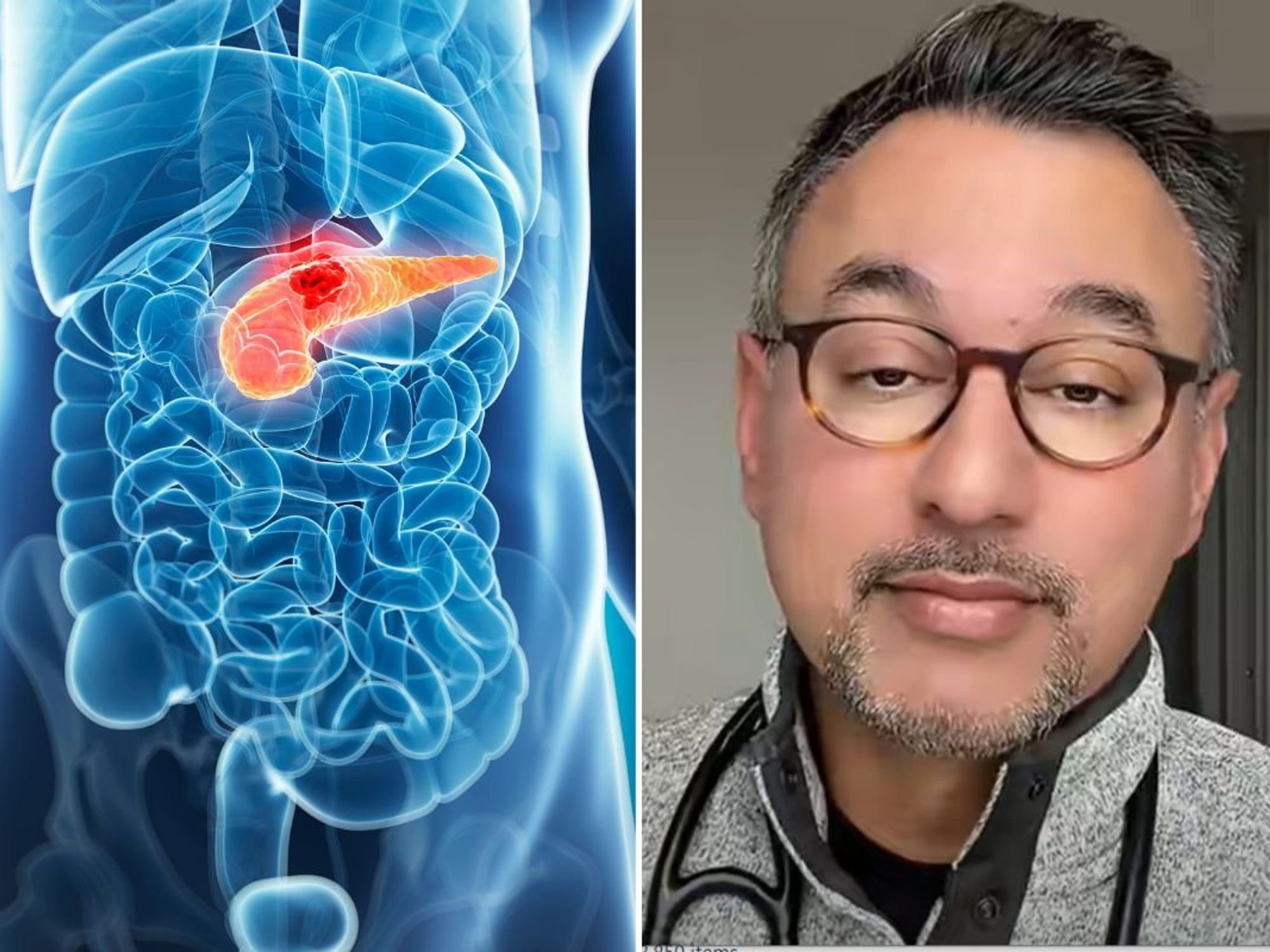
Doctor Q&A: Are antibiotics secretly killing me? Doctor Renée answers your burning health questions

Celebrity NHS doctor Renée Hoenderkamp addresses GB News members' burning questions
|Doctor Renée Hoenderkamp

In this week's Q&A, celebrity NHS Doctor Renée Hoenderkamp breaks down the potential side effects of antibiotics, recovery hacks for a stomach bug and how to get moving again after a hip replacement
Don't Miss
Most Read
There's a yawning gap between what our intuitions tell us about our health and what "the science" tells us.
This can lead us to make counterintuitive decisions, such as over-medicalising common ailments.
Thankfully, doctors can help bridge the gap between intuition and practical advice.
The questions submitted to Doctor Renée Hoenderkamp via health@gbnews.uk for this week's Doctor's Q&A are a powerful reminder of the importance of deferring to medical opinion.
Doctor Hoenderkamp sheds light on the hidden health risks posed by antibiotics, how to speed up recovery from a stomach bug and how to regain fitness after a hip replacement
Last week, our resident doc revealed the worst foods for eye health, how to remedy heartburn and the underlying causes of poor gut health.
It's important to remember that the advice given below is general and not individual and you should always seek individualised health care from a doctor.
With those caveats aside, see below Doctor Hoenderkamp's answers to GB News members' burning questions.
Hey doctor Renee I have seen you say often that you try and never take antibiotics but my GP seems to give them to me whenever I go. Why don't you like them?
Hey doctor Renee I have seen you say often that you try and never take antibiotics but my GP seems to give them to me whenever I go. Why don't you like them?
It’s not that I ‘don’t like’ antibiotics, it’s that I don’t like the side effects and I don’t want to use an antibiotic and have to live with the side effects if I don’t need them. I also feel that in the majority of cases when we give adults and children antibiotics, we don’t need them, we are treating a virus, so when there is no role for an antibiotic, all we get are all the down sides for no up!
So, breaking down what those effects are:
Gut microbiome
This is one of the most important parts of our immune system. Eighty per cent of our immune cells are in our gut and healthy gut bacteria help build up the immune system. When you take an antibiotic, you wipe out your gut microbiome for up to two years! Why do that if it isn’t needed and put yourself on the back foot when it comes to tackling viral and bacterial infections in the future?
Diarrhoea, nausea, vomiting, rashes
One in five people will get side effects that include one of these side effects, amongst others. Why have any side effects if it isn’t needed?
Resistance
Every time an antibiotic is used, there is the potential for it to kill some of the particular bacteria but leave those more hardy ones behind. This then allows the bacteria in question to strengthen against the antibiotic until eventually that antibiotic will not work against the bacteria it was designed to kill. This has seen the emergence of ‘superbugs’ which kill people. In 2019, 2.1 million people worldwide died from an antibiotic resistant bacteria. The fewer antibiotics we use as a society and personally, the less chance of this happening. If we continue to overuse antibiotics we will potentially reach a point in time where cutting yourself in the garden will be fatal. No one wants to go back to those dark days.
One of the most common reasons I get asked for an antibiotic by a patient is for a cough/cold/chest infection that has dragged on for a week or so. The first problem with this is that most people just don’t realise that a cold will take 10-14 days to resolve and the cough that you are often left with, can persist for six to eight weeks quite normally. What I do when someone insists on an antibiotic, and they don’t have a clear clinical indication for it, is offer them a chest X-ray – if there is a lower respiratory infection on X-ray then antibiotics are needed. I have audited this over a winter cold season and less than five per cent of patients asking for an antibiotic actually needed one! This is because most colds and coughs, however bad they appear, are viruses, and there is nothing an antibiotic will do against a virus.
I hope that explains my position and I promise I do practise what I preach.
Hey Doctor Renée, what do you recommend for speeding up recovery for a stomach bug. Anything that I could be missing? There's one going around at the moment and I've definitely caught it. Thanks
There is certainly a stomach bug or two going around at the moment and the symptoms can vary from nausea and loss of appetite all the way through to vomiting and diarrhoea. The first thing to say is that if you have severe stomach pain and a temperature with vomiting, always speak to your doctor; you don’t want to miss appendicitis!
However, if you are sure it’s an infectious bug (for example if other people around you have it too) then there are some things that you can do to help speed up the healing process or give it a helping hand.
Firstly, I always advise people to cut dairy out of their diet completely for a couple of weeks (and remember dairy is in many processed food including biscuits). The reason for this is that when our gut is upset by a bacteria causing a tummy bug, you can get a transient lactose intolerance and if you eat dairy it can just prolong things. So take the dairy out, let the gut heal and reintroduce it slowly. If symptoms flare up, take it out for a further couple of weeks and repeat.
Make a gut-soothing home remedy to help calm the irritated gut lining and replace electrolytes Cut a four-inch piece of peeled ginger into thin slices and simmer in one litre of water for 15 minutes. Sieve and allow to cool. Add the juice of three lemons and half a teaspoon of sea salt. Have one to two cups per day, cold or warmed.
This should keep in the fridge for up to two days.
Take a good probiotic to encourage the replenishment of your good bacteria and see the bad off. I always recommend Symprove, it’s the one I take.
Reintroduce food slowly eating little and often and keep things simple. Go for good quality, fresh food, cooked at home and avoid too many fatty snacks.
It’s a simple approach but it should help and continuing with the pro-biotic should help you fend off the next bug!
Hey Renée, three months ago I had a hip replacement. I am desperate to get moving again. What exercises do you recommend to get me back into shape? Thank you
Recovery after major surgery can take time and some effort, especially when dealing with a joint such as the hip that is so critical in movement and supports much of body weight. Recovery is also very dependent on you, the patient, and will change with age and underlying fitness and medical conditions and the type of surgery you have.
You should have had some post-surgery physiotherapy and have some exercises to do at home. These will be personalised to you and the type of surgery you have had so it is impossible for me to suggest particular exercises. However, I can give some pointers.
You say that you are three months in but taking you back to the weeks leading up to three months, the pain and swelling should be decreasing and mobility improving. Your physiotherapy will continue to focus on enhancing strength, endurance, and stability. The best activities now are walking, swimming and low-impact exercises.
By three months, most people experience significant improvements in mobility and reduced pain and should be able to resume normal activities. This should include higher-impact exercises and sports but if you are not there yet, don’t push it. Physiotherapy focus, if continuing, should be on maintaining strength, flexibility, and optimising joint function. It’s important to gradually reintroduce daily activities such as driving, work, and household chores as advised by your surgeon and follow their guidelines on what and when.
But if you are not at or near this point, don’t despair, as I said, progress will vary dramatically from person to person and it can take up to a year to be fully restored to normal. However, if you haven’t had physio or are unsure what exercises you should be doing, please contact your surgical team and ask for some rehabilitation.
There is also a good video here with pre and post-surgery exercise that may help but don’t do anything that is painful and seek advice from your surgical team.
Good luck.